AVM (Arteriovenous Malformation)
Understanding Causes, Symptoms, and Treatment Options
What is AVM?
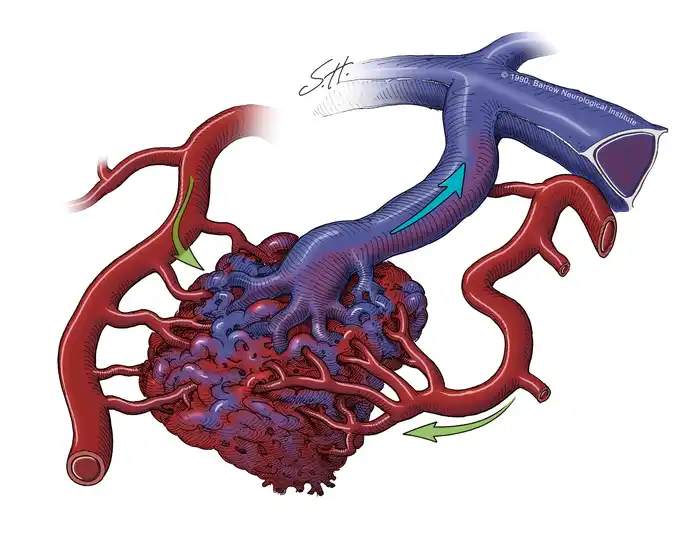
Arteriovenous Malformation (AVM) is a rare condition involving an abnormal tangle of arteries and veins, bypassing the capillary system. This disrupts normal blood flow and oxygen delivery, often leading to complications such as hemorrhage or neurological symptoms. AVMs can occur in various parts of the body, including the brain, spine, and other organs.
Key Features of AVM
- Abnormal connection between arteries and veins
- High blood flow and pressure in the affected vessels
- Potential risk of rupture, causing internal bleeding
- Commonly congenital, though sometimes diagnosed later in life
Symptoms of AVM
Symptoms vary depending on the location and severity of the AVM. Common symptoms include:
- Headaches or migraines
- Seizures
- Neurological symptoms like weakness or numbness
- Vision or speech disturbances
- Hearing a pulsating noise in the head (bruit)
- Sudden severe symptoms if the AVM ruptures, such as stroke-like symptoms
Causes and Risk Factors
The exact cause of AVM is unknown, but it is believed to occur during fetal development. Risk factors include:
- Congenital: Most AVMs are present at birth
- Family History: Rare genetic mutations may increase risk
- Gender: Some studies suggest a slight prevalence in males
- Age: Often detected between the ages of 10 and 40
How is AVM Diagnosed and Treated?
Diagnosis involves imaging studies to identify the size, location, and risk of the AVM:
- CT or MRI: Provides detailed images of the brain and AVM
- Angiography: Uses contrast dye to map blood flow through the AVM
- Ultrasound: Identifies AVMs in other parts of the body
Treatment options vary based on the AVM's size, location, and risk of complications:
- Observation: Small, asymptomatic AVMs may only require monitoring.
- Endovascular Embolization: A minimally invasive procedure where a catheter is used to block abnormal vessels with glue, coils, or other materials.
- Stereotactic Radiosurgery (SRS): Focused radiation to shrink the AVM over time.
- Open Surgery: Direct removal of the AVM, often used for accessible and high-risk lesions.
Risks and Potential Complications
If untreated, AVMs can lead to serious complications, such as:
- Hemorrhage: Rupture of the AVM can cause life-threatening bleeding
- Neurological Damage: Pressure on surrounding brain tissues can impair function
- Seizures: Resulting from abnormal electrical activity in the brain
- Stroke: Due to disrupted blood flow or AVM rupture
Recovery and Long-Term Management
Patients can improve outcomes with:
- Regular follow-up imaging to monitor AVM size and risk
- Adhering to prescribed treatment plans
- Managing risk factors such as high blood pressure
- Engaging in physical therapy or rehabilitation, if needed
With timely treatment and monitoring, many patients achieve symptom relief and reduce the risk of complications.